Wound Charting: A Complete Information for Nurses
Associated Articles: Wound Charting: A Complete Information for Nurses
Introduction
With nice pleasure, we are going to discover the intriguing matter associated to Wound Charting: A Complete Information for Nurses. Let’s weave attention-grabbing data and supply recent views to the readers.
Desk of Content material
Wound Charting: A Complete Information for Nurses
Wound care is a vital side of nursing observe, requiring meticulous consideration to element and correct documentation. Wound charting, an important part of this course of, serves a number of functions: it supplies a transparent document of the wound’s development (or regression), guides therapy choices, facilitates communication amongst healthcare professionals, and helps authorized and high quality assurance necessities. This text supplies a complete overview of wound charting for nurses, encompassing greatest practices, important components, and customary challenges.
The Significance of Correct Wound Charting
Correct and constant wound charting is paramount for a number of causes:
-
Monitoring Wound Therapeutic: Common charting permits for the target monitoring of wound therapeutic. By documenting adjustments in measurement, depth, exudate, and surrounding tissue, nurses can assess the effectiveness of the present therapy plan and make well timed changes. This longitudinal document supplies essential information for evaluating therapy efficacy and figuring out potential issues.
-
Early Detection of Issues: Detailed wound charting may also help establish early indicators of an infection, dehiscence (wound separation), or different issues. Modifications in odor, elevated ache, purulent drainage, or indicators of systemic an infection (fever, tachycardia) ought to be promptly documented and reported. Early detection considerably improves affected person outcomes and reduces morbidity.
-
Improved Communication: A well-maintained wound chart serves as a transparent and concise communication device amongst healthcare suppliers. Physicians, nurses, wound care specialists, and different members of the interdisciplinary group can readily entry the data wanted to coordinate care and guarantee consistency in therapy. That is notably essential in conditions involving affected person transfers or consultations.
-
Authorized Safety: Thorough and correct wound charting supplies authorized safety for nurses. Within the occasion of a authorized declare, the wound chart serves as an important piece of proof demonstrating the standard of care offered and the rationale behind therapy choices. Incomplete or inaccurate charting can have critical authorized implications.
-
High quality Assurance and Analysis: Information collected by wound charting contributes to high quality assurance initiatives and analysis research. Evaluation of wound chart information may also help establish areas for enchancment in wound care protocols, monitor the effectiveness of various therapy modalities, and contribute to the event of evidence-based practices.
Important Components of a Wound Chart
A complete wound chart ought to embrace the next data:
-
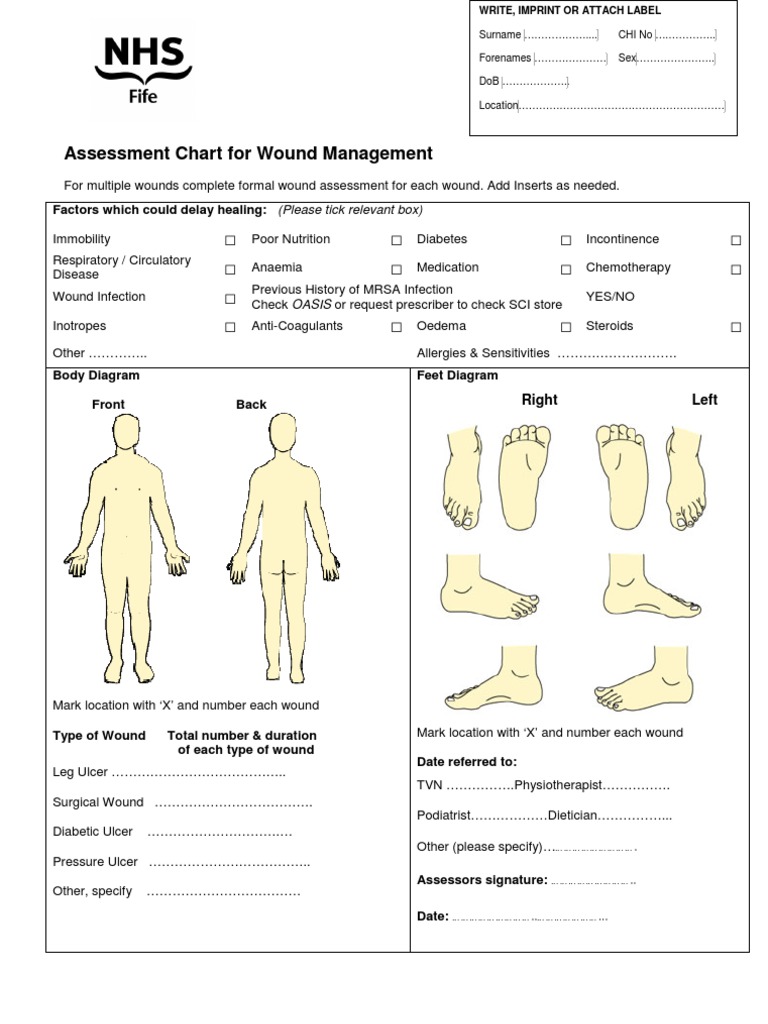
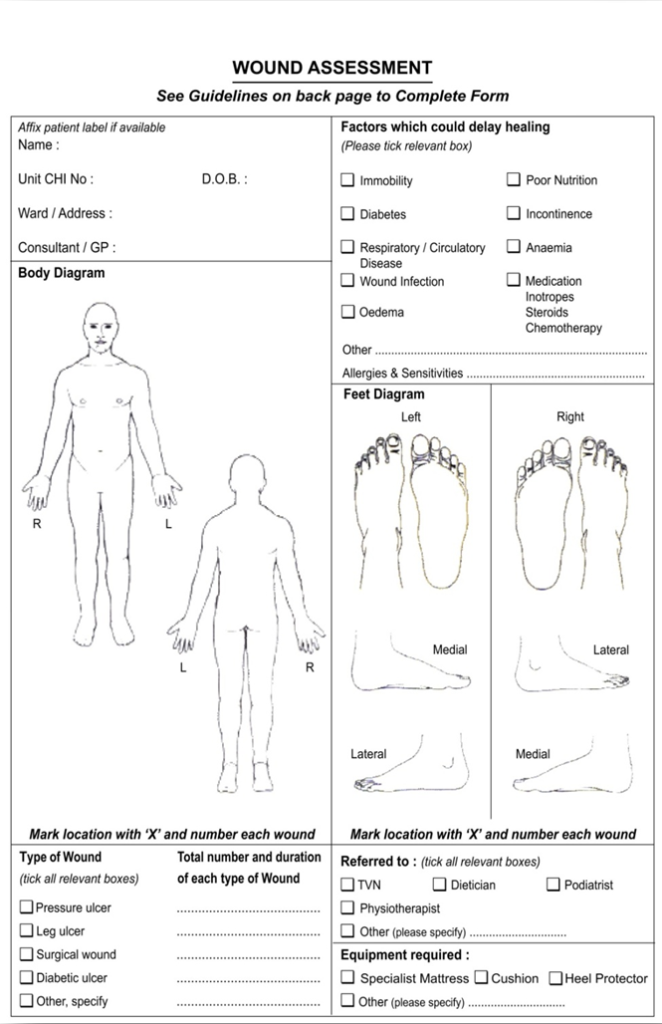
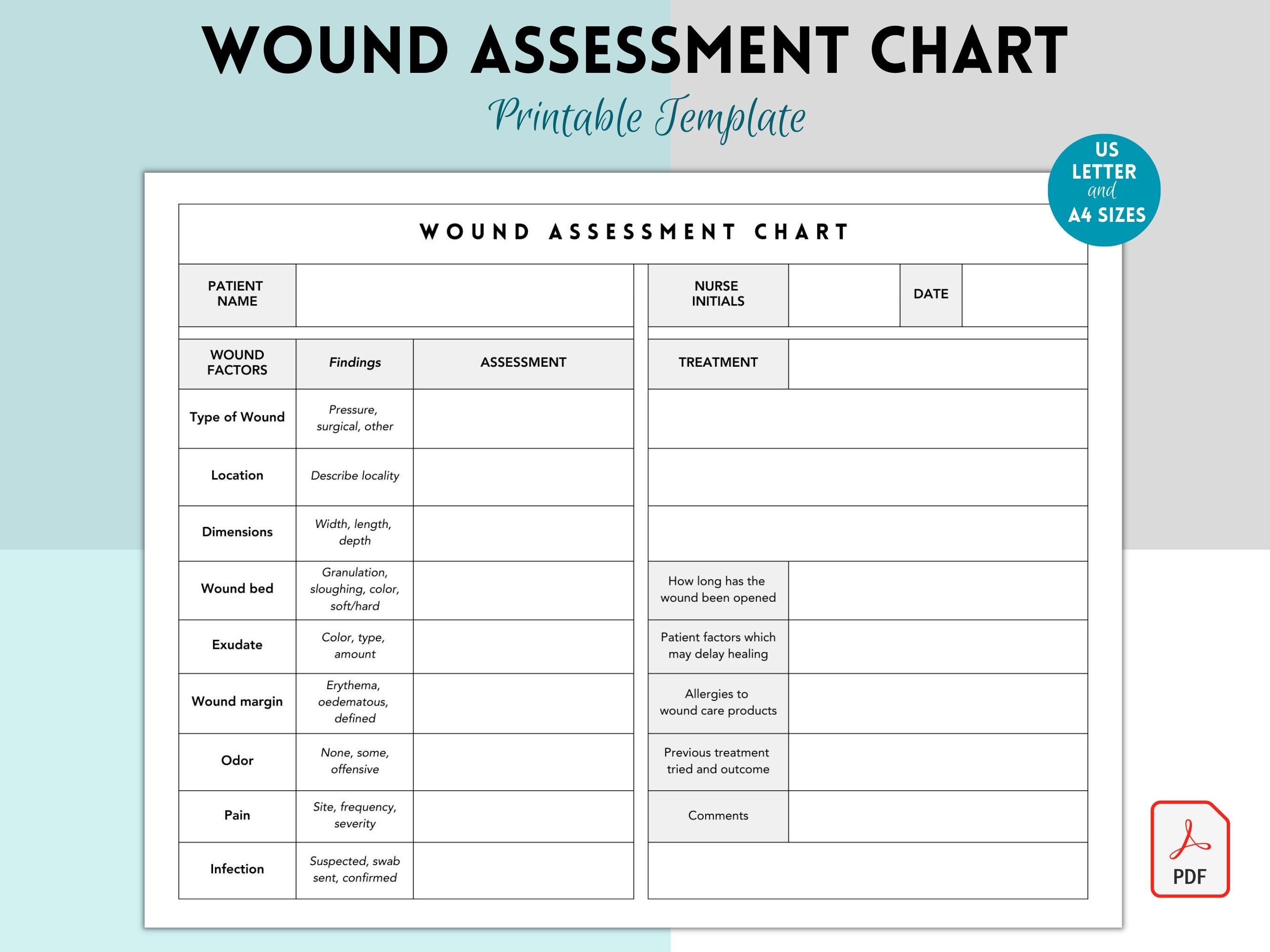
Affected person Identification: This contains the affected person’s full title, medical document quantity, date of start, and different related identifiers.
-
Date and Time: Every wound evaluation ought to be clearly timestamped to make sure correct monitoring of adjustments over time.
-
Wound Location: Exactly describe the placement of the wound utilizing anatomical landmarks (e.g., "2 cm superior to the medial malleolus of the suitable leg").
-
Wound Measurement: Measure the wound in centimeters utilizing size, width, and depth. For irregular wounds, a number of measurements could also be essential. Use standardized strategies to make sure consistency.
-
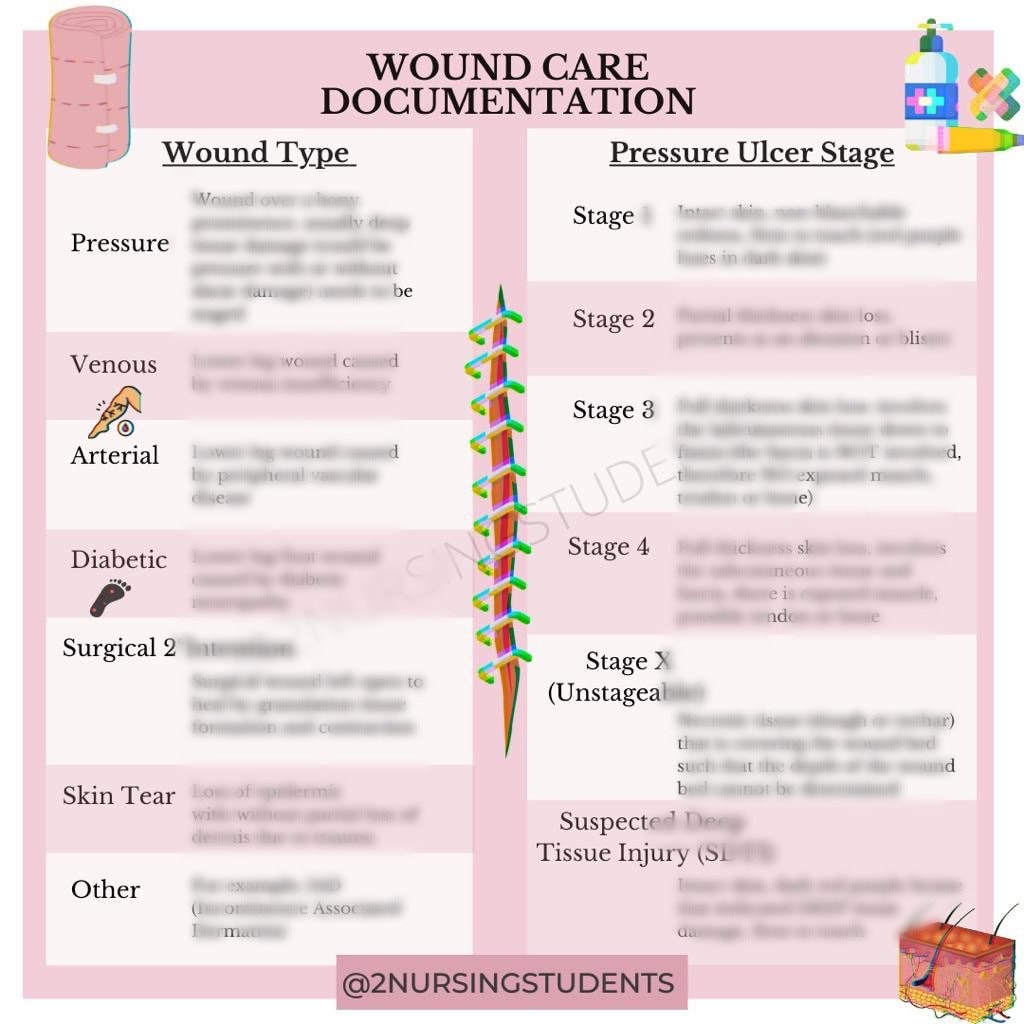
Wound Kind: Doc the kind of wound (e.g., strain ulcer, surgical wound, traumatic wound, venous ulcer, arterial ulcer, diabetic ulcer). Embody the stage of a strain ulcer in keeping with the suitable staging system (e.g., NPUAP/EPUAP staging system).
-
Wound Mattress Look: Describe the looks of the wound mattress, noting the presence of granulation tissue (wholesome, pink tissue), slough (yellow or tan, stringy tissue), eschar (black, necrotic tissue), or fibrin (a yellowish-white movie).
-
Wound Edges: Describe the situation of the wound edges, noting whether or not they’re well-approximated, everted, undermined, or rolled.
-
Exudate: Doc the quantity, shade, consistency, and odor of wound exudate. Use descriptive phrases akin to scant, average, or copious; serous (clear, watery), serosanguineous (pinkish), sanguineous (bloody), or purulent (pus).
-
Periwound Pores and skin: Assess the situation of the pores and skin surrounding the wound, noting any erythema (redness), edema (swelling), induration (hardening), maceration (softening), or blistering.
-
Ache Evaluation: Use a standardized ache scale (e.g., numerical score scale, visible analog scale) to doc the affected person’s ache degree associated to the wound.
-
Remedy: Doc all wound care interventions, together with dressings used, frequency of dressing adjustments, topical drugs utilized, and another related remedies.
-
Affected person Training: Document any affected person schooling offered relating to wound care, together with directions for dressing adjustments, hygiene, and indicators and signs of an infection.
-
Affected person Response to Remedy: Doc the affected person’s response to the therapy, noting any enhancements or antagonistic results.
-
Images: Digital pictures could be a beneficial addition to the wound chart, offering visible documentation of the wound’s look over time. Receive knowledgeable consent from the affected person earlier than taking any pictures.
Frequent Challenges in Wound Charting
Nurses could encounter a number of challenges in wound charting:
-
Inconsistent Terminology: Utilizing inconsistent terminology can result in misinterpretations and hinder efficient communication. Utilizing standardized terminology and definitions is essential.
-
Time Constraints: Busy scientific environments could make it difficult to dedicate adequate time to thorough wound charting. Prioritizing correct documentation is important regardless of time pressures.
-
Lack of Coaching: Insufficient coaching in wound evaluation and documentation can result in inaccurate or incomplete charting. Common persevering with schooling and coaching are essential.
-
Subjective vs. Goal Information: It is essential to distinguish between subjective (patient-reported) and goal (observable) information. Whereas each are essential, goal information ought to be prioritized in wound charting.
-
Digital Well being Information (EHRs): Whereas EHRs supply many advantages, they will additionally current challenges, akin to difficulties in navigating the system, restricted house for detailed descriptions, and potential for information entry errors.
Finest Practices for Wound Charting
-
Use a Standardized Format: Make use of a standardized wound charting format to make sure consistency and completeness.
-
Be Particular and Goal: Use exact language and keep away from imprecise phrases. Give attention to observable information somewhat than interpretations.
-
Use Correct Measurements: Make use of standardized measurement strategies to make sure accuracy and comparability of wound measurement over time.
-
Keep Common Charting: Chart wound assessments commonly, in keeping with the established care plan.
-
Evaluate and Replace: Frequently overview and replace the wound chart to replicate any adjustments within the wound’s situation or therapy plan.
-
Collaborate with the Interdisciplinary Workforce: Work collaboratively with different healthcare professionals to make sure constant and complete wound care.
-
Make the most of Know-how: Discover using digital wound charting techniques and digital pictures to enhance effectivity and accuracy.
Conclusion
Wound charting is a basic side of offering high-quality wound care. Correct, constant, and complete documentation is important for monitoring wound therapeutic, detecting issues, facilitating communication, making certain authorized safety, and contributing to high quality enchancment initiatives. By adhering to greatest practices and overcoming frequent challenges, nurses can play a significant position in optimizing affected person outcomes by efficient wound administration and meticulous wound charting. Steady schooling and adherence to standardized tips are essential for sustaining the best requirements of wound care documentation.
![20100728 Wound Assessment Tool Guide Final[2] 287](http://image.slidesharecdn.com/3c80de9e-a70c-4984-a340-b57a7b841cd4-150129125750-conversion-gate01/95/20100728woundassessmenttoolguidefinal2-2-638.jpg?cb=1422557894)




Closure
Thus, we hope this text has offered beneficial insights into Wound Charting: A Complete Information for Nurses. We admire your consideration to our article. See you in our subsequent article!